Minimum pricing isn't working
Public health campaigners are baffled. The public, not so much.
Minimum pricing of alcohol in Scotland is not going well. Self-styled public health advocates are baffled.
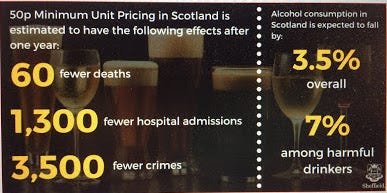
Now in its fifth year and facing a sunset clause next year, the Scottish government’s own evaluation has made grim reading for those who claimed that setting a floor price of 50p on a unit of alcohol would be a game-changer in Scotland’s relationship with The Drink.
In October 2021, the evaluation of the impact of minimum pricing on crime found…
.. no changes in the trend direction or statistically significant changes in the level of all alcohol-related crime and disorder
(Except in one local authority where alcohol-related crime went up.)
In the same month, a thorough evaluation of the impact of minimum pricing on alcohol-related A & E attendances was published. It found that the policy may have been associated with an increase in visits:
The odds ratio for an alcohol-related emergency department attendance following minimum unit pricing was 1.14 (95% confidence interval 0.90 to 1.44; p = 0.272). In absolute terms, we estimated that minimum unit pricing was associated with 258 more alcohol-related emergency department visits (95% confidence interval –191 to 707) across Scotland than would have been the case had minimum unit pricing not been implemented.
In June 2022, the evaluation looked at the heavy drinkers who were supposed to benefit most from minimum pricing. Its conclusions were unflinching:
There is no clear evidence that MUP led to an overall reduction in alcohol consumption among people drinking at harmful levels or those with alcohol dependence, although some individuals did report reducing their consumption.
People drinking at harmful levels who struggled to afford the higher prices arising from MUP coped by using, and often intensifying, strategies they were familiar with from previous periods when alcohol was unaffordable for them. These strategies typically included obtaining extra money, while reducing alcohol consumption was a last resort.
MUP led to increased financial strain for a substantial minority of those with alcohol dependence as they obtained extra money via methods including reduced spending on food and utility bills, increased borrowing from family, friends or pawnbrokers, running down savings or other capital, and using foodbanks or other forms of charity.
Some people with alcohol dependence and their family members reported concerns about increased intoxication after they switched to consuming spirits rather than cider. In some of these cases, people also expressed concerns about increased violence.
Alcohol-related hospital admissions refused to decline after the policy was introduced and alcohol-related deaths are at a nine-year high, although lockdowns doubtless had an affect on the latter. The policy cost Scottish drinkers £270 million in its first four years and all the SNP have to cling to is a modest drop in alcohol consumption, much of which is due to COVID-19.
Last month, a new piece of research was published in BMJ Open looking at alcohol consumption. It was not part of the official evaluation and was produced by academics who are very sympathetic to minimum pricing. They nevertheless struggled to make the policy look like a success.
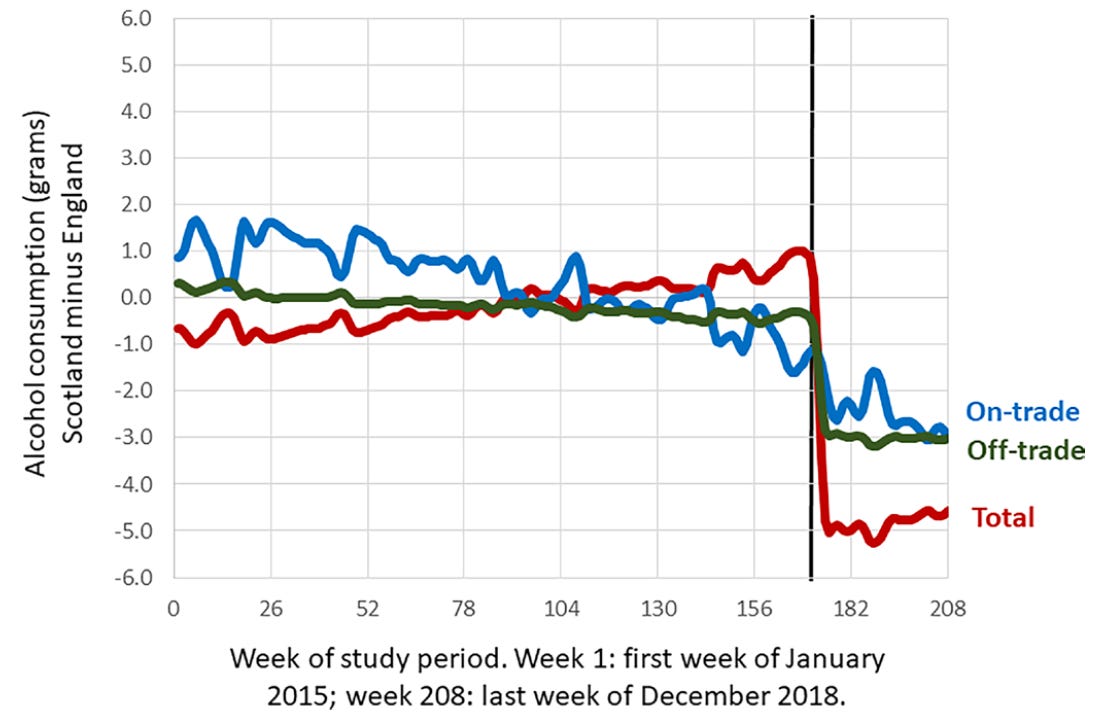
Using Kantar survey data and comparing Scotland to northern England, they found that the introduction of minimum pricing was followed by a drop in consumption, as shown below.
It looks like an impressively steep decline until you realise that 5 grams of alcohol is barely half a unit. Per week. And the reduction in consumption from the off-trade, which is the only place minimum pricing makes any difference, was just 3 grams.
Moreover, the reduction in consumption was not evenly spread across the population. It was weighted towards women who tend to drink less anyway.
The reductions in consumption are largely driven by women (a reduction of 8.6 g per week, 95% CI 2.9 to 14.3) rather than by men (a reduction of 3.3 g per week, 95% CI –3.6 to 10.4)
And among men who were the heaviest drinkers, consumption actually increased.
For the 95th percentile the introduction of MUP was associated with an increase in consumption for men of 13.8 g (95% CI 5.8 to 21.5), but not for women (4.8 g, 95% CI −4.0 to 13.7).
The study also contains bad news for the pub industry which, in classic Baptists and bootleggers fashion, supported minimum pricing for nakedly self-interested reasons.
For younger men there was an increase in off-trade consumption, which was offset by decreases in on-trade consumption in the same group.
I warned that this would happen five years ago. Leave people with less money in their pocket and they will have less to spend on the luxuries in life, like going to the pub.
None of these findings are terribly surprising to people who are more worldly than your average ‘public health’ academic. Raising the price of cheap booze was always more likely to change the behaviour of moderate tipplers than heavy drinkers. Hardcore drinkers were always going to find money to keep drinking and minimum pricing was never going to help the pub trade. It was only likely to make the poor poorer.
The authors of the study seem flabbergasted that a policy that had so much (naive and flawed) modelling behind it could turn out like it has.
When the Minister for Public Health, Sport and Wellbeing introduced the 2018 alcohol policy framework, he emphasised that the implementation of the MUP [minimum unit price] was strongly motivated by an interest in decreasing health inequalities through a reduction in alcohol consumption among the heaviest and most vulnerable drinkers. Our results indicate that this goal may not be fully realised…
You can say that again.
… first, we found that women, who are less heavy drinkers in our data and in almost all surveys worldwide to date, reduced their consumption more than men; second, the 5% of heaviest drinking men had an increase in consumption associated with MUP; and, third, younger men and men living in more deprived areas had no decrease in consumption associated with MUP. These results are surprising as modelling studies would have suggested otherwise.
It takes a heart of stone not to laugh at the best laid plans of philosopher kings falling apart at the seams.
We do not know why, for both younger men (those aged <32 years) and for those living in residential areas in the bottom two-fifths of deprivation, there was no decrease in consumption associated with MUP compared with older men and those living in less deprived areas.
One wonders if the authors have ever met any men aged under 32 or anyone in the bottom two-fifths of the income distribution.
Several studies have found that overall, heavier drinkers— including people with alcohol use disorders—react less to price than the general population (ie, they react more price inelastic and their consumption is determined by other factors). However, while this may explain lower reductions, it cannot explain an increase in consumption.
Yes, that is a particularly awkward finding. Even I didn’t see that coming.
The results may also imply a diminished impact on alcohol-attributable hospitalisations and mortality, which have been shown to be strongly associated with heavy drinking in men and in those of lower socioeconomic status. Indeed, a large controlled study on emergency department visits following the introduction of MUP did not show any reduction in alcohol-related emergency department visits.
It’s fair to say that minimum pricing hasn’t gone the way that the likes of Dr Nick Sheron, a blowhard anti-alcohol campaigner, expected. In 2014, he insisted that minimum pricing was an ‘almost perfect alcohol policy because it targets cheap booze bought by very heavy drinkers and leaves moderate drinkers completely unaffected’. In the same year, Sir Ian Gilmore, chair of the Alcohol Health Alliance, described minimum pricing as an ‘evidence-based policy exquisitely targeted at those, and those around them, who are currently suffering harm’.
In a sensational act of hubris, three activist-academics published an article in 2017 claiming that the evidence-base for minimum pricing, a policy that had never been tried anywhere, fulfilled the great epidemiologist Austin Bradford Hill’s criteria for causality. It seemed absurd at the time and it seems almost grotesque now.
Still, this being ‘public health’, the answer to the medicine failing is to demand more of the same medicine.
If indeed the findings of our study are corroborated, then additional and/or different pricing mechanisms may need to be considered to reduce alcohol-attributable hospitalisations and mortality.
‘Tis but a flesh wound!
Postscript
While I was writing this post, I came across this new study which finds evidence of another unintended consequence which seems obvious to the man on the Clapham omnibus but never occurred to those who have qualifications in public health.
Following the introduction of MUP, total household food expenditure in Scotland declined by 1.0%, 95%CI [-1.9%, − 0.0%], and total food volume declined by 0.8%, 95%CI [-1.7%, 0.2%] compared to the north of England.
That might not necessarily be a bad thing. Scotland has an obesity problem, after all.
There is variation in response between product categories, with less spending on fruit and vegetables and increased spending on crisps and snacks.
Oh.


Minimum pricing meant I stopped buying locally and went to Amazon or increasingly to Spain for booze. In order to justify the effort of an online Spanish order and reduce shipping cost, it means making big orders. With more booze sitting about the house, do I drink more - its hard to say, not much but probably yes. I always have some to hand, its not as if I will finish a bottle and think, -right that's it until I go shopping on Saturday.
Ironically, since Brexit, booze from Spain has become cheaper. The Spaniards refund Spanish VAT, and UK customs don't bother to charge any duty or VAT, so long as you keep the order below approx £100. Three out of four deliveries don't get checked, one in four gets inspected, delayed a fortnight, but still delivered without charge.
And yes I barely go to pubs any more. The smoking ban, the covid nonsense of masks when you stand up, one way systems to go to the bog etc, general nanny statism, put me and it seems other off. Reduced footfall equals higher prices and a spiral of cutting back social drinking, but more spare cash for buying nicer stuff at home (not bought locally).
All MUP has done is impoverish alcoholics. Aren't there people in alcohol policymaking who want to actually help people suffering from a devastating disease, rather than just protect progressive shibboleths?